I have been totally slacking in the blog department. But it's not because I have a lack of medical material to report about these days. Nope. Quite the opposite in fact. The last 3 months I have had more appointments and tests than I ever have had before.
I have always had bad eyes. Like everyone in my family, I am near-sighted. I started wearing glasses for distance in about the 6th grade to see the board in school. Eventually my vision worsened enough that I started needing glasses all the time and once I got old enough I transitioned into contact lenses. Over the years, I had a pretty good system where I went to the optometrist every other year and reordered my one year prescription of contacts and managed to make them last (in combination of wearing my glasses) until my next appointment.
In September, I went for a routine eye exam with my optometrist. I felt like my eyes had worsened and probably needed a new prescription. However, I expected to be in and out of the appointment fairly quickly, with the outcome resulting in an up-to-date prescription that would allow me to order fresh new contact lenses. Unfortunately, this wasn't in the cards.
While the optometrist was checking my eyes he noticed that the vision in my left eye was not improving with a higher prescription. This is actually my least favorite part of the appointment when the eye doctor says over and over, "Which is better: 1...2...1...2?" I have always had a hard time with that. After my eyes dilated, upon examination he noticed that there were "shiny spots" on my left macula compared to my right macula. This prompted him to refer me to an ophthalmologist within the next week. He said, "Sorry it wasn't a 'See you next year!' appointment."
I went to see an ophthalmologist named Dr. C who did a field test and a optical coherance tomography (OTC) scan. The tests were normal (apart from two small cycles in the parafoveal of my left eye) and upon examination she did not see anything wrong with my macula. She said to return for an appointment in about 3 months.
About a 3-4 weeks later, I noticed my vision started to get whacky. I felt like I couldn't see my computer very well and the words on the screen were missing letters or parts of letters. I noticed this also while driving and reading highway signs. I called Dr. C and she recommended coming in for an appointment. She repeated the OTC scan which then showed bilateral cystoid macular edema.
A normal OCT - less than 250 microns.
My left eye in November - 571 microns.
My right eye in November - 465 microns.
See those big holes? Yeah. Not good.
My opthalmologist was a bit shocked, and actually questioned if I was the right patient and wondered if there had been some sort of mix up with the tech who performed the OCT scan. Unfortunately...no mix up!
I returned to the office a few days later and had a fluorescein angiography - a test that revealed bilateral retinal vasculitis. Retinal vasculitis can be idiopathic or it can be caused by an infectious or autoimmune process. The first step was to rule out any type of infection that could be causing the retinal vasculitis. The first-line treatment for retinal vasculitis that is not caused by infection is prednisone, but that would be contraindicated if the retinal vasculitis were caused by infection. I was tested for a million different things and during that time my vision reduced to 20/40. Scary.
No infectious cause was found and I was prescribed prednisone. Steriods. Roid rage. The prescription was for 50 mg daily and was told to taper by 10 mg each week for a total of about 5-6 weeks.
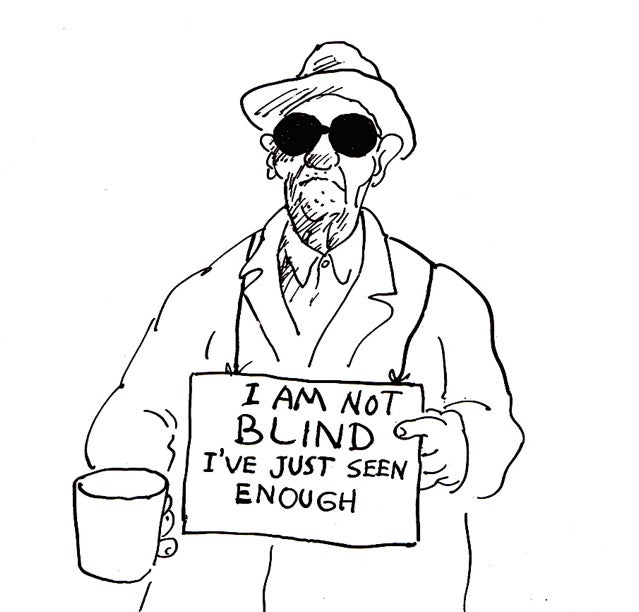
Of course, I turned to google and began researching retinal vasculitis, a "sight threatening condition". A lot of very scary things can cause retinal vasculitis. Then, I began researching prednisone. Mood swings. Weight gain. Irritability. Anxiety. Moon face. Diabetes. Bone loss. Ahhhhh. The alternative? Blindness.
My thoughts exactly.
And so began a 3 month adventure consisting of rheumatology, neurology, and myelomology appointments and evaluations.
And just to make things a tad more exciting...
Prednisone is evil.



.JPG)
.JPG)